By Asha Bekidusa | abekidusa@gmail.com
The Kenyan coast is witnessing increased interventions on malaria, amid growing concerns over climate change-driven health challenges seen to worsen infant mortality and maternal morbidity.
According to a recent spatial analysis published in “Science Direct”, 11 per cent of all malaria cases in Kenya are concentrated in coastal endemic areas, necessitating urgent targeted interventions.
More data from the region shows the country’s Kwale County with the highest disease burden, followed by Kilifi then Mombasa.
“In Kwale, malaria remains a leading cause of under-five mortality and maternal morbidity, as children and pregnant women are affected most. Malaria is no longer just a health issue, but a climate justice issue,” says Eva Muthuuri, Malaria Representative of the Global Fund’s Kenya Coordinating Mechanism (KCM) and a member of the End Malaria Council and Fund.
Ms Muthuri says their data reflects the climate-driven shift in disease burden of malaria.
Strengthening Community Partnership and Empowerment (SCOPE) CEO Jasho Bomu says communities living near abandoned mining areas are at most risk of malaria, as the areas are easy breeding ground for mosquitoes.
He encourages rehabilitation of mining areas, especially in Kwale and Kilifi counties, where a lot of mining happens and quarries are abandoned.
Margaret Mundia, a Health Systems Specialist at Global Fund KCM, says collaboration between stakeholders is key in combating malaria.
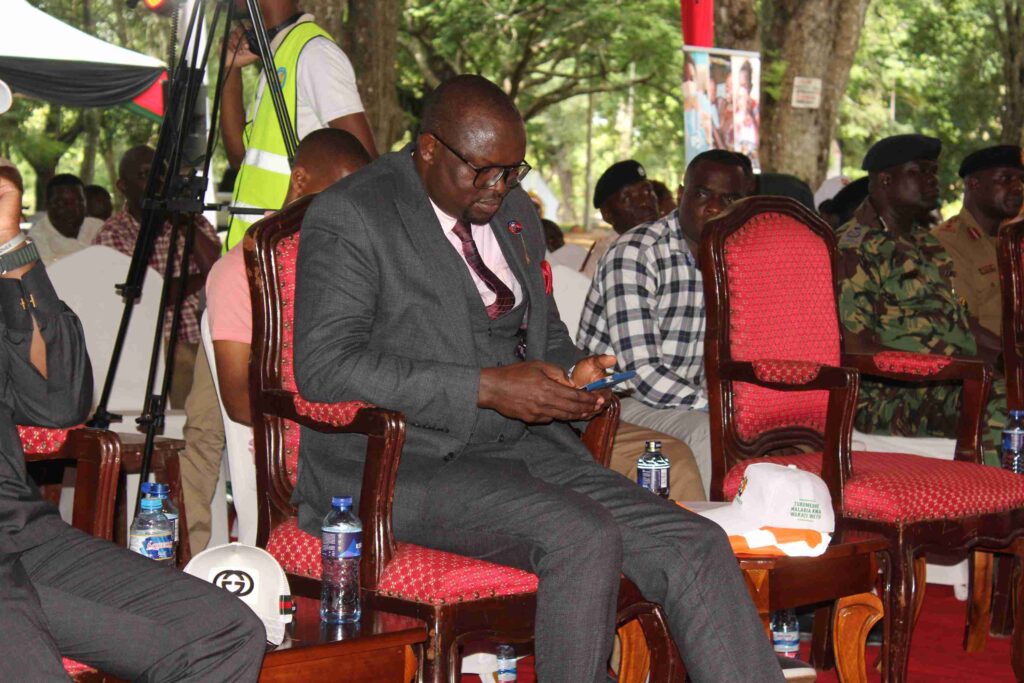
Speaking during the commemoration of World Malaria Day on April 25, Roneek Vora, a member of the End Malaria Council said the recent suspension of US foreign aid, including USAID and the President’s Malaria Initiative, had created Ksh25 billion (about $194 million) funding gap in Kenya’s national malaria response, posing real danger to gains made and systems that sustain the efforts.
Vora is also the Director of Sales and Marketing at Revital Healthcare.
He highlighted the importance of the private sector’s role in fighting malaria by establishing local efforts such as manufacturing facilities to produce kits to help fight malaria.
“We’ve established Africa’s largest rapid diagnostic test (RDT) manufacturing facility, capable of producing 20 million kits monthly,” he said.
At the same event in Kwale, Gilbert Wangalwa, the AMREF Deputy Country Director in Kenya, appealed for cross boundary collaborations between counties and countries in dealing with malaria.
He mentioned African countries such as Algeria, Cabo Verde, Lesotho, Mauritius, Morocco and Seychelles, as having political goodwill to be declared malaria free by World Health Organisation.
Mr Wangalwa sought better use of data, technology and Artificial Intelligence to power localised response for targeted intervention in malaria hotspots.
Director of Preventive and Promotive Healthcare at Kenya’s Ministry of Health, Dr Lenai Joseph, said during the same commemorations that hotspots were concentrated in counties surrounding Lake Victoria, Turkana, and Kwale.
“Over 70 per cent of our population remains at risk,” said Dr Lenai, adding: “Malaria continues to hinder our socio-economic development, keeping children out of school, reducing productivity and increasing household healthcare costs.”
Despite the disease burden, Dr Lenai highlighted that malaria prevalence had dropped nationally from 8 per cent to 6 per cent over the last decade. He said malaria incidences had dropped from 112 per 1,000 in 2016, to 84 per 1,000 population by end of 2024.
He said this overall progress in Malaria Control had contributed to the reduction of infant, child and maternal mortality nationally.
At the same event, the Kwale Deputy Governor Chirema Kombo vowed to work together with all stakeholders in the fight against Malaria.

The 2025 theme, Malaria Ends with Us: Reinvest, Reimagine, Reignite encourages discussion of innovative strategies and addressing persistent challenges in the fight against malaria particularly in East Africa.
Kenya, Tanzania, and Uganda who occupy this region and who all border Lake Victoria – together accounted for nearly 10 per cent of malaria cases worldwide in 2022, with an estimated 23.8 million cases and upwards of 53,000 deaths.